Specialist's Corner
Living with nonalcoholic fatty liver disease
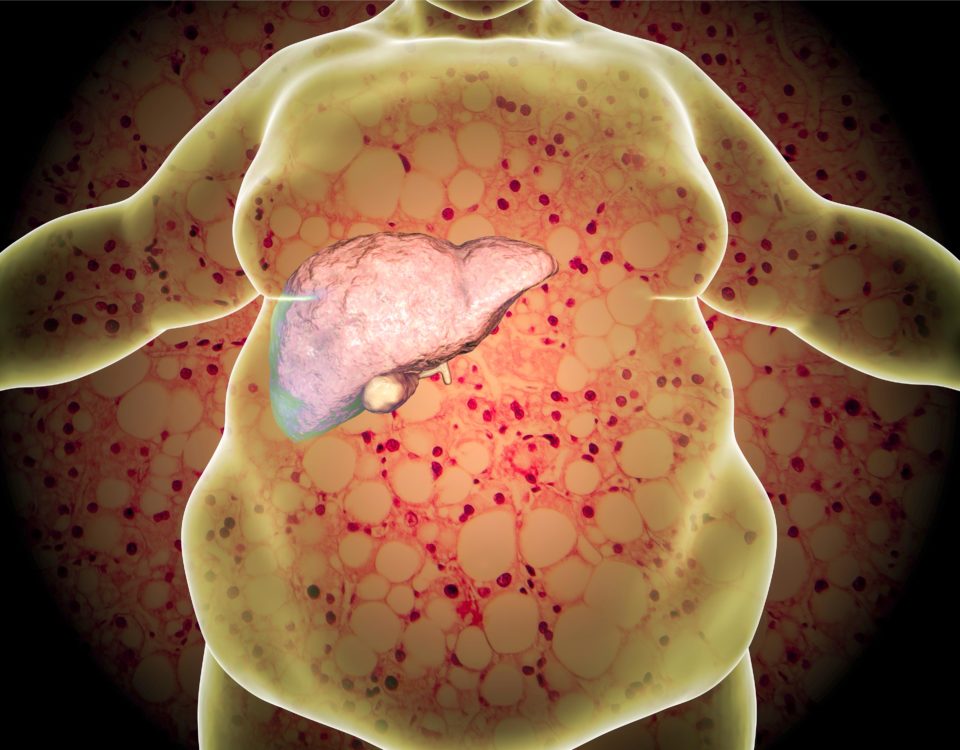
Nonalcoholic fatty liver disease (NAFLD) is the build up of extra fat in liver cells that is not caused by alcohol. It is normal for the liver to contain some fat. However, if more than 5% – 10% percent of the liver’s weight is fat, then it is called a fatty liver (steatosis). The development of nonalcoholic fatty liver disease is intimately associated with and is probably caused by obesity and diabetes although sometimes it occurs in individuals who are neither obese nor diabetic. Nonalcoholic fatty liver disease is a manifestation of an abnormality of metabolism within the liver. The liver is an important organ in the metabolism (handling) of fat. The liver makes and exports fat to other parts of the body. It also removes fat from the blood that has been released by other tissues in the body, for example, by fat cells, or absorbed from the food we eat. In nonalcoholic fatty liver disease, the handling of fat by liver cells is disturbed. Increased amounts of fat are removed from the blood and/or are produced by liver cells, and not enough is disposed of or exported by the cells. As a result, fat accumulates in the liver.
Nonalcoholic fatty liver disease can be divided into isolated fatty liver in which there is only accumulation of fat, and nonalcoholic steatohepatitis (NASH) in which there is fat, inflammation, and damage to liver cells. Usually, to differentiate isolated fatty liver from NASH requires a liver biopsy The most promising treatments for nonalcoholic fatty liver disease are diet, exercise, weight loss, and possibly bariatric surgery. Several drugs have been studied in the treatment of NASH. There is little evidence that any drug is effective in slowing the disease progression.
Symptoms of fatty liver disease
Fatty liver disease rarely causes symptoms until the liver disease is far advanced. When the liver disease is far advanced (cirrhosis), signs and symptoms of cirrhosis predominate. These include: Excessive bleeding due to the inability of the liver to make blood-clotting proteins; Jaundice due to the inability of the liver to eliminate bilirubin from the blood; Gastrointestinal bleeding due to portal hypertension that increases the pressure in intestinal blood vessels; Fluid accumulation due to portal hypertension that causes fluid to leak from blood vessels and the inability of the liver to make the major blood protein, albumin, and mental changes (encephalopathy) due to the liver's inability to eliminate chemicals from the body that are toxic to the brain. Other causes of nonalcoholic fatty liver disease include Wilson's disease, lipodystrophy (a disease of fat storage), starvation, intravenous nutrition, and abetalipoproteinemia (a disease of fat transport). Several drugs also cause nonalcoholic fatty liver disease, for example cortilcosteroids, tamoxifen (Nolvadex), and methotrexate.
Can obesity and diabetes cause NASH?
Obesity and diabetes have important roles in the development of fatty liver. Whereas one third of the general population (which includes obese and people with diabetes) may develop nonalcoholic fatty liver disease, more than two thirds of people with diabetes develop nonalcoholic fatty liver disease. Among patients who are very obese and undergoing surgery for their obesity, the majority have nonalcoholic fatty liver disease. Moreover, whereas the risk of NASH is less than 5% among lean persons, the risk is more than a third among the obese.
Can metabolic syndrome cause NASH?
Metabolic syndrome is a syndrome defined by the association of several metabolic abnormalities that are believed to have a common cause. These metabolic abnormalities result in obesity, elevated blood triglycerides, low density lipoprotein (LDL or "bad" cholesterol) and high density lipoprotein (HDL) cholesterol, high blood pressure, and elevated blood sugar (diabetes). Nonalcoholic fatty liver disease is considered a manifestation of metabolic syndrome and thus occurs frequently with the other manifestations of the syndrome. Occasionally, it may occur without the other abnormalities of the syndrome.
Can NASH occur in children?
Since the current epidemic of obesity begins in childhood, it is not surprising to find that nonalcoholic fatty liver disease occurs in children. Only a few studies are available, but the estimated prevalence among children 2-19 years of age is approximately 10%, the prevalence increases with the degree of obesity, and there is progression to cirrhosis. It is recommended, however, that children with suspected nonalcoholic fatty liver disease in whom the diagnosis is not clear should have a liver biopsy. Children should not be started on any drug treatment for nonalcoholic fatty liver disease without a biopsy showing NASH. Although there have not been studies in children to support the recommendations, loss of weight and exercise are the recommended treatment for children with nonalcoholic fatty liver disease.
Prevention & treatment
Treatment for nonalcoholic fatty liver disease includes lifestyle changes (exercise, weight loss, diet), medications, supplements and antioxidants, Omega-3 fatty acids, surgery, and liver transplantation. Nonalcoholic fatty liver disease has been associated in human or animal studies with reduced amounts of unsaturated fats (a diet high in saturated fat) and increased amounts of fructose (which is most commonly added to the diet as high-fructose corn syrup). Benefits of increasing unsaturated fat (a diet lower in saturated fat, and higher unsaturated fat) and reducing high fructose corn syrup on nonalcoholic fatty liver disease have not been demonstrated; however, there is little harm in doing so, especially since there may be benefits of these dietary modifications unrelated to the liver. An interesting observation - though unexplained - is that there is less scarring (fibrosis) in the livers of patients with NASH who drink more than two cups of coffee per day (Scarring or fibrosis is the process that ultimately leads to cirrhosis). Similar benefits of coffee have been associated with lesser degrees of liver disease in both alcoholic cirrhosis and hepatitis C. It is not unreasonable to recommend drinking coffee in moderate amounts in view of the lack of harmful side effects. Vitamin D deficiency is associated with nonalcoholic fatty liver disease. Although there is no reason to think that this deficiency contributes to nonalcoholic fatty liver disease, it is reasonable to measure vitamin D levels in patients with nonalcoholic fatty liver disease and treat them with vitamin D if they are deficient. Since the serious complications of nonalcoholic fatty liver disease are primarily seen in patients with NASH, treatment of NASH is of great importance. Unfortunately, there are no clearly effective treatments for these patients. One of the difficulties in identifying effective treatments is the need for long-term studies since the progression of NASH to cirrhosis and its complications occurs slowly. Several treatments have resulted in a reduction of fat in the liver, but few have shown that the progression of NASH is slowed. Weight loss and exercise are among the most promising of treatments for nonalcoholic fatty liver disease. It does not take large amounts of weight loss to result in a decrease in liver fat. A less than 10% decrease in weight may be enough. Vigorous exercise results in a reduction of liver fat and may reduce the inflammation of NASH. The long-term effects of weight loss and exercise on the important development of cirrhosis and its complications are unknown. Nevertheless, now, the best theoretical approach to nonalcoholic fatty liver disease is weight loss and vigorous exercise. Unfortunately, only a minority of patients are able to accomplish these. There are no drugs that are approved for the treatment of fatty liver or NASH.














Leave a comment