Specialist’s Corner
Dr Deepak K Agarwal
The writer is senior consultant gastroenterologist, hepatologist & endoscopist and is running a successful medical Centre in Lucknow
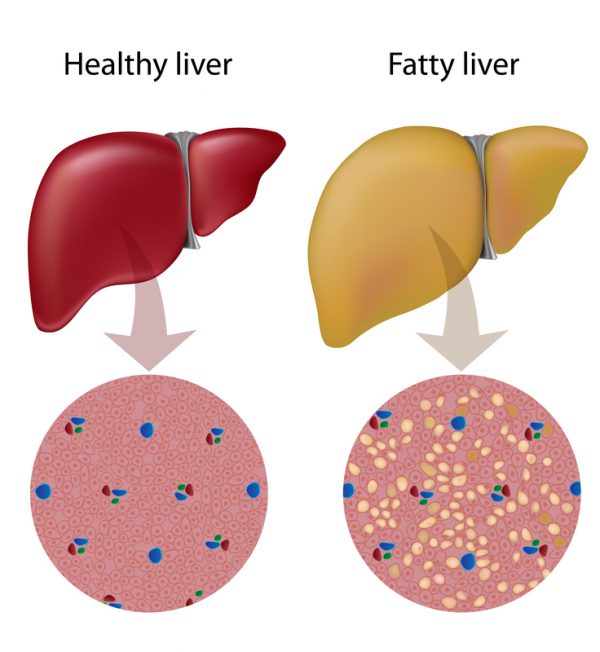
Your liver is the second largest organ in your body. It helps process nutrients from food and drinks, and filters harmful substances from your blood. Too much fat in your liver can cause liver inflammation, which can damage your liver and create scarring. In severe cases, this scarring can lead to liver failure. Fatty liver disease is a common condition caused by the storage of extra fat in the liver. Most people have no symptoms, and it doesn’t cause serious problems for them. In some cases, though, it can lead to liver damage. The good news is you can often prevent or even reverse fatty liver disease with lifestyle changes. Fatty liver is also known as hepatic steatosis. A healthy liver contains a small amount of fat. It becomes a problem when fat reaches 5% to 10% of your liver’s weight.
When fatty liver develops in someone who drinks a lot of alcohol, it is known as alcoholic fatty liver disease (AFLD). In someone who does not drink a lot of alcohol, it is known as non-alcoholic fatty liver disease (NAFLD). In most cases, fatty liver disease doesn’t cause any serious problems or prevent your liver from functioning normally. But for 7% to 30% of people with the condition, fatty liver disease gets worse over time. It progresses through three stages: Your liver becomes inflamed (swollen), which damages its tissue. This stage is called steatohepatitis. Scar tissue forms where your liver is damaged. This process is called fibrosis. Extensive scar tissue replaces healthy tissue. At this point, you have cirrhosis of the liver. Cirrhosis of the liver is a result of severe damage to the liver. The hard scar tissue that replaces healthy liver tissue slows down the liver’s functioning. Eventually, it can block liver function entirely. Cirrhosis can lead to liver failure and liver cancer.
You have a greater chance of developing fatty liver disease if you: are of Hispanic or Asian descent; have completed menopause (your periods have stopped); have obesity with a high level of belly fat; have high blood pressure, diabetes or high cholesterol and/or have obstructive sleep apnea (a blocked airway that causes breathing to stop and start during sleep). Some people get fatty liver disease without having any pre-existing conditions. But these risk factors make you more likely to develop it: Having overweight/obesity; having Type 2 diabetes or insulin resistance; having metabolic syndrome (insulin resistance, high blood pressure, high cholesterol and high triglyceride levels), or taking certain prescription medications, such as amiodarone, diltiazem, tamoxifen or steroids.
People with fatty liver disease often have no symptoms until the disease progresses to cirrhosis of the liver. If you do have symptoms, they may include: Abdominal pain or a feeling of fullness in the upper right side of the abdomen (belly); nausea, loss of appetite or weight loss; yellowish skin and whites of the eyes (jaundice); swollen abdomen and legs (edema); extreme tiredness or mental confusion, or weakness. Fatty liver can progress through four stages, including: Simple fatty liver: There is a build-up of excess fat in the liver. Simple fatty liver is largely harmless if it doesn’t progress. Steatohepatitis: In addition to excess fat, there’s also inflammation in the liver. Fibrosis: Persistent inflammation in the liver has now caused scarring. However, the liver can still generally function normally. Cirrhosis: Scarring of the liver has become widespread, impairing the liver’s ability to function. This is the most severe stage and is irreversible. Both AFLD and NAFLD present similarly. Fatty liver condition is assigned a grading system to determine the severity of the condition. This is necessary to provide better treatment plans for a rapid recovery. Grade I – simple form that does not interfere with the proper functioning of the liver, but still requires to be managed. Grade II – a middle condition that requires some medical help to prevent its progression. Grade III – a severe state of the disease. It is usually at this stage that symptoms appear.
There is no medication specifically for fatty liver disease. Instead, doctors focus on helping you manage factors that contribute to the condition. They also recommend making lifestyle changes that can significantly improve your health. So far, the two best drug options affirmed by the American Association for the Study of Liver Diseases for biopsy-proven NASH are vitamin E (an antioxidant) and pioglitazone (used to treat diabetes). However, not everyone will benefit from these treatments, and there has been some concern about safety and side effects. If you have NASH, it is best to speak to your doctor about whether these treatments are appropriate for you, as they are not for everyone. There are more drugs in the pipeline, some with promising initial study results. So, the treatment includes: avoiding alcohol; losing weight; taking medications to manage diabetes, cholesterol and triglycerides (fat in the blood); taking vitamin E and thiazolidinediones (drugs used to treat diabetes) in specific instances, and following a balanced diet to lose weight slowly but steadily. Rapid weight loss can actually make fatty liver disease worse. Doctors often recommend the Mediterranean diet, which is high in vegetables, fruits and good fats.
The good news is that the most effective treatment so far for fatty liver disease does not involve medications, but rather lifestyle changes. The bad news is that these are typically hard to achieve and maintain for many people. Here's what we know helps: Lose weight. Weight loss of roughly 5% of your body weight might be enough to improve abnormal liver tests and decrease the fat in the liver. Losing between 7% and 10% of body weight seems to decrease the amount of inflammation and injury to liver cells, and it may even reverse some of the damage of fibrosis. Target a gradual weight loss of 1 to 2 pounds per week, as very rapid weight loss may worsen inflammation and fibrosis. You may want to explore the option of weight loss surgery with your doctor, if you aren't making any headway with weight loss and your health is suffering. It appears that aerobic exercise and gym also leads to decreased fat in the liver, and with vigorous intensity, possibly also decreased inflammation independent of weight loss. Eat well. Some studies suggest that the Mediterranean diet may also decrease the fat in the liver. This nutrition plan emphasizes fruits, vegetables, whole grains, legumes, nuts, replacing butter with olive or canola oil, limiting red meat, and eating more fish and lean poultry. Drink coffee, maybe? Some studies showed that patients with NAFLD who drank coffee (about two cups every day) had a decreased risk in fibrosis. However, take into consideration the downsides of regular caffeine intake. Even though it can be difficult to make these lifestyle changes and lose the weight, the benefit is immense if you have fatty liver, so give it your best effort! And remember, the greatest risk for people with a fatty liver is still cardiovascular disease. Not only can some of these lifestyle changes improve or resolve your fatty liver, they will also help keep your heart healthy.













Leave a comment